

So far, classifications of MS subtypes have been based largely on clinical phenomenology, but there is growing evidence that the subgroups of MS also differ with respect to epidemiology, pathogenesis, genetics, neuropathology, and neuroimaging. The aim of this study was investigating a possible role of β endorphin in the mechanisms leading to different clinical expressions of MS. As in other autoimmune diseases (such as rheumatoid arthritis and Crohn’s disease), β endorphin concentrations are decreased in MS. 4Īs is the case for other autoimmune diseases, MS is supposed to result from an imbalance between proinflammatory and anti-inflammatory factors. Moreover, the concentrations of PBMC β endorphin in the present group of controls was comparable with those found in other groups of controls. This group of controls was very well matched with the patients in terms of age and sex, and their health condition was carefully checked to rule out any past or ongoing disease. The results of this study confirm our previous data 4 showing reduced β endorphin concentrations in the immune cells of patients with MS compared with controls. Correlations were evaluated with the Pearson product moment correlation. 7ĭifferences in β endorphin concentrations were analysed by analysis of variance, followed by post hoc Bonferroni corrected t test. The presence and number of gadolinium enhanced lesions were assessed by an experienced observer following published guidelines.
Β ENDORPHIN FULL
Images were acquired with a 1.5 T scanner, with full brain coverage (the scan geometry was 24 contiguous, axial, 5 mm thick slices with approximately 1 × 1 mm in-plane pixel resolution).
In 39 patients, dual echo spin-echo and post-contrast (intravenous gadolinium-DTPA, 0.1 mmol/kg) T1 weighted spin-echo magnetic resonance images of the brain were also obtained within 48 hours after blood sample collection. Sensitivity of the method was 10 pg per tube, and intra-assay and interassay variation coefficients were 8% and 11 % respectively.

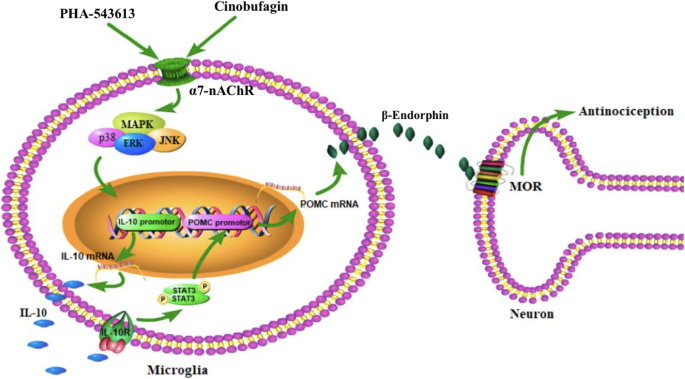
4 The antiserum used was directed to the C terminal sequence of human β endorphin. 4 The antiserum and radiommunoassay procedures to measure β endorphin were previously described and validated. Supernatants were frozen for radioimmunoassay. Cells were resuspended in 1 ml of 0.1 normal acetic acid, homogenised, and centrifuged. Aprotinin (Boehringer Ingelheim Pharmaceutical Inc, Ridgefield, Connecticut, USA) 1000 kIU was added to all samples before storage at −20° to inhibit peptide degradation. In all patients and controls, peripheral blood samples were collected in a tube containing EDTA, and PBMC were separated by gradient sedimentation over Ficoll-Paque (Pharmacia, Uppsala, Sweden). Β Endorphin concentrations were also measured in 12 healthy controls (five men and seven women) with a mean (SD) age of 40.0 (4.4) years. Patients experiencing relapses started steroid treatment after blood sample collection None of the patients had ever taken disease modifying treatments (such as interferons, glatiramer acetate, mithoxantrone) or were being treated with neuroleptic, antidepressant, or antiepileptic drugs. To this end, we measured β endorphin concentrations in PBMC from patients with MS with clinically different phenotypes or in different phases of the disease. 4 In this study, we investigated the possible role of β endorphin in determining the heterogeneity of the course of MS. We found reduced concentrations of PBMC β endorphin in patients compared with healthy controls, increased concentrations of β endorphin during interferon beta treatment compared with basal values, and increased concentrations of β endorphin soon after a clinical relapse. 5 We have previously evaluated β endorphin concentrations in peripheral blood mononuclear cells (PBMC) of patients with MS. 4 β Endorphin is synthesised by cells of the central nervous system (arcuate nucleus) and immune system (lymphocytes, thymocytes, monocytes, and splenocytes). 3 Among non-conventional immune mediators, the opioid peptide β endorphin has been shown to affect some immune responses, which in turn modulate cytokine production. Several studies have shown a pronounced increase of Th1 cytokines in patients with active disease, 2 whereas interleukin 10, transforming growth factor β, and interleukin 4 have been found to be downregulated during phases of disease activity and upregulated during phases of disease remission. The immunological mechanisms of multiple sclerosis (MS) are only partially defined, but they are known to differ between patients and in different phases of the disease.


 0 kommentar(er)
0 kommentar(er)
